Safe Sex

What is safe sex?
Safe sex is a set of practices and approaches to reduce the risk of contracting sexually transmitted infections (STIs) and prevent unwanted pregnancy; where the main goal of these practices is to protect the health of both partners. It is important to understand that even if all the rules are followed, the risk cannot be completely eliminated, but it can be significantly minimized.
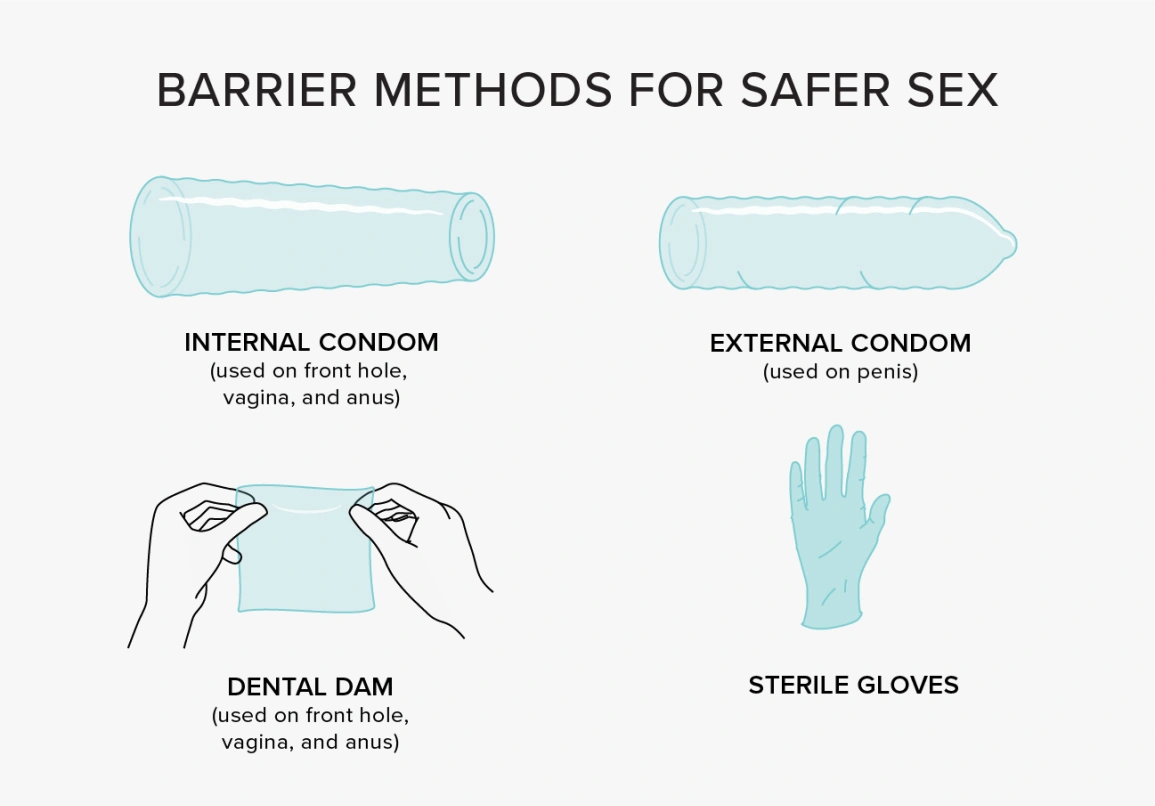
Condoms and other barrier methods: how to choose and use them correctly
People commonly use condoms to prevent sexually transmitted infections together with unwanted pregnancy, because they remain both practical and inexpensive. The standard method of condom use contains subtle factors which need your understanding for proper protection results.
The first thing to look at is the material. Most often condoms are made of latex: it stretches well, is reliable and suitable for most people. But if you are allergic to latex, it is better to choose a version of polyurethane or polyisoprene - they also effectively protect and do not cause irritation.
The second important point is the size, as a condom that is too small can tear, and a condom that is too big can slip off at the most inopportune moment. So do not take the first one you find, especially if there are problems with comfort or density; the right size means both reliability and pleasant sensations.
It is very important to put on a condom before any contact between the genitals, because infections can be transmitted not only through semen, but also through mucous membranes. When putting it on, make sure there is no air in the reservoir at the end - otherwise it can inflate and cause it to tear. After sex, the condom should be carefully removed, tied so that its contents don't leak out, and thrown in the trash - not the toilet.

Additional measures for safe sex : from contraceptive choices to new technologies
When it comes to safer sex, it is important to realize that there is no one-size-fits-all solution; in this sense, protection methods are selected individually, depending on health, age, lifestyle and personal preferences. For example, hormonal means - pills, patches, injections - do an excellent job of preventing pregnancy, but do not protect against infections. Therefore, they are often combined with barrier methods, especially when it comes to new or irregular partners.
Some women opt for an intrauterine device - it is convenient, long-lasting and with a high degree of protection against pregnancy. But before installation, it is necessary to consult with a doctor, because this method is not suitable for everyone and may have limitations for medical reasons.
Modern medicine does not stand still, and every year there are new ways to protect yourself. For example, antiviral gels and microbicides are being actively developed - they are applied to mucous membranes before sex to further reduce the risk of infection with HIV and other viruses. While these products are not yet a substitute for condoms, they are already considered a good additional level of protection, especially in high-risk settings.
Another interesting development is a new generation of condoms made of innovative materials such as graphene, which is both very strong, flexible and virtually insusceptible. These “hybrid” condoms promise a high level of comfort and reliability, but for now they are still undergoing trials before being mass-produced.
Tests and check-ups: why you need regular STI screenings
One of the basics of safe sex is not only protection, but also regular medical testing, as many sexually transmitted infections may not manifest themselves for a long time. Without symptoms, a person may not even realize that he or she is a carrier and can infect a partner; therefore, preventive check-ups are not just a formality, but a way to really protect yourself and others.
If you have one regular partner and the relationship is monogamous, it is reasonable to get tested at least once a year; but if you have an active sexual life with several partners, you should be tested more often - every 3-4 months. This is not only about HIV and syphilis, but also about such things as chlamydia, gonorrhea, mycoplasmosis, herpes and other STIs.
Medical diagnosis requires multiple blood or urine tests to achieve proper identification of health conditions. On the other hand, extended medical testing with PCR detection is more beneficial because it lets you identify DNA pathogens at their earliest infection stage.
How to make oral and anal sex safer
Oral sex is not as harmless as it may seem: it can also transmit infections, including herpes, gonorrhea, syphilis and other STIs. Therefore, to reduce the risks, it's a good idea to use barrier protection. For example, for cunnilingus, special latex films (dental dams) are suitable, and for fellatio - ordinary condoms; which are simple and affordable ways to protect yourself, especially when contacting new or untested partners.
Anal sex requires even more attention to safety. Lack of anal lubrication makes tissue damage possible due to the absence of vaginal fluid, and these microcracks are a direct route to infection. Using a quality condom with the right lubricant (water or silicone-based) can help avoid injury and significantly reduce the risk of transmitting infections, including HIV.
Intimate hygiene: how to take care of yourself without harming your health
Taking care of the intimate area is an important part of preventive care and sexual health. Before sex, many people use special products - whether it's mouthwashes or mild intimate hygiene gels. This helps reduce the chances of transmitting bacteria and infections, especially when it comes to oral sex.
But it's important not to overdo it here, because aggressive antiseptics, soaps with strong fragrances or antibacterial gels can disrupt the natural balance of microflora, dry out the mucosa and cause irritation. All this only increases the risk of infection, not reduces it. Therefore, the selection of products with a neutral pH value along with no detectable odors, serves as a better choice than those containing aggressive components.
The microbiome and sexual health: what the science says
Modern research increasingly suggests that the genital microbiome - that is, the collection of “your own” microorganisms living on the mucosa - plays a key role in sexual and reproductive health. When this internal ecosystem is healthy, it protects against infections, helps maintain natural pH levels, and prevents harmful bacteria from multiplying. But on the other hand, when the ecosystem is out of balance, the risk of disease - such as bacterial vaginosis, candidiasis, and other STIs - increases.
To keep the microbiome normal, it is important not to destroy it with aggressive means. In this sense, for hygiene soft products without flavorings and antiseptics are suitable, as they do not wash out the beneficial bacteria and do not dry out the mucosa. It is also worth being careful with antibiotics: with frequent use, they kill not only pathogens, but also the necessary microbes, breaking the body's natural defenses.
Lubricants also affect the microfloral; therefore, it is better to choose those that do not contain aggressive preservatives and alcohol components - especially if you are prone to irritation or dryness. Remember, the more you take care of your microflora, the less likely you are to experience inflammation, infections and other problems.
How alcohol and drugs affect sexual behavior
When alcohol or psychoactive substances come into play, the ability to make a sober assessment of the situation decreases dramatically. This also applies to sex: under the influence of alcohol or drugs, people are more likely to refuse condoms, ignore risks and make decisions that they later regret.
When intoxicated, it's easy to lose control, forget to protect yourself, or fail to notice signals that something is going wrong. All of this increases the likelihood of contracting STIs and sometimes sexual encounters that a sober person would not have agreed to.
To stay conscious and act in your best interest, it's best to avoid alcohol and substances before safe sex, or at least control the amount.
Modern prevention methods: vaccines and drugs against infections
Safe sex is not just about condoms. Today, medicine offers more comprehensive approaches to protection, including vaccinations and special drugs that reduce the risk of contracting dangerous infections.
Vaccination against HPV (human papillomavirus) and hepatitis B is one of the most effective forms of long-term prevention. These viruses can be sexually transmitted and can cause serious complications over time, including cervical, liver and other cancers. Therefore, vaccinations are especially important for those who are new to sexual activity or have multiple partners, but are also suitable for adults - especially if they have not been vaccinated before.
HIV prevention with PrEP and PEP deserves special attention. PrEP is pre-exposure prophylaxis, in which a person takes medication in advance to protect themselves in case of possible exposure to the virus. The risk stands highest among people who share their lives with an HIV-positive partner or who face high exposure to the virus. While PEP functions for prevention after one experienced unprotected sexual contact with someone who might transmit HIV infection. The medication must be initiated as quickly as possible to achieve its best effect and this critical time period should fall within 72 hours.

FAQ`s
Can I wear two condoms for more protection?
At first glance it seems logical: two condoms means twice the protection; but in practice, the opposite is true. Using two condoms at the same time - whether two male condoms or two male and female condoms together - increases the risk that they will break. It's all about friction between the layers: it creates additional stress and can damage the material.So it's better to use one condom, but correctly: choose the right size, make sure the package is intact, don't use expired products and don't forget about lubrication if necessary.
When comparing male and female condoms, which option provides better reliability and what sets them apart from each other?
Placing the male condom over an erect penis stands opposite to the placement method of the female condom which goes inside the vagina before securing the ends with rings. The male and female condom work identically for STI prevention and they prevent unintended pregnancies.In terms of effectiveness, they are about equal if used correctly, so the difference is mainly one of feel and convenience. For example, the female condom can be inserted in advance - several hours before intimacy, which is convenient if you don't want to interrupt the moment. Some people note that the female version feels different during sex and may be more comfortable in certain situations.
What signs can indicate the presence of an STI?
Sexually transmitted infections often make themselves known through symptoms such as genital itching, burning, rash, unusual discharge, foul odor or pain during urination. Sometimes there is pain during sex or discomfort in the lower abdomen.But most importantly, many STIs can be completely asymptomatic. This means that a person can be a carrier of the infection and not even realize it, continuing to pass it on to others.
Do hormonal contraceptives protect against STIs?
Hormonal methods - pills, injections, implants or spirals - do a good job of preventing pregnancy, but they do not protect against sexually transmitted infections. None of these forms of contraception creates a barrier between partners' bodies, so viruses and bacteria are easily transmitted through sexual contact.To reduce the risk of contracting an STI, hormonal methods should be combined with condoms or other barrier methods. Only this combination can protect against both unwanted pregnancies and infections.

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/